Abstract
Introduction
Central venous catheters (CVC) are necessary for medically complex and acutely ill children, but come with the risk of venous thromboembolism (VTE) or central line associated blood stream infection (CLABSI). The rate of VTE in pediatrics has increased, most likely due to the increased use and placement of CVCs, and questions remain regarding VTE risk factors for CVC associated thrombosis.
Methods
This prospective, multi-center study compared the incidence and risk factors for VTE between peripherally inserted central catheters (PICCs) and centrally inserted tunneled lines (TLs) in patients 6 months to <18 years from 4 pediatric hospitals from September 2013 to April 2018. Data were collected through medical record review regarding demographics, medical history and specific CVC data including insertion technique and catheter specifications. Subjects were prospectively monitored via medical record review for CVC complications including VTE, CLABSI or malfunction (use of tissue plasminogen activator, malposition, blockage, etc).
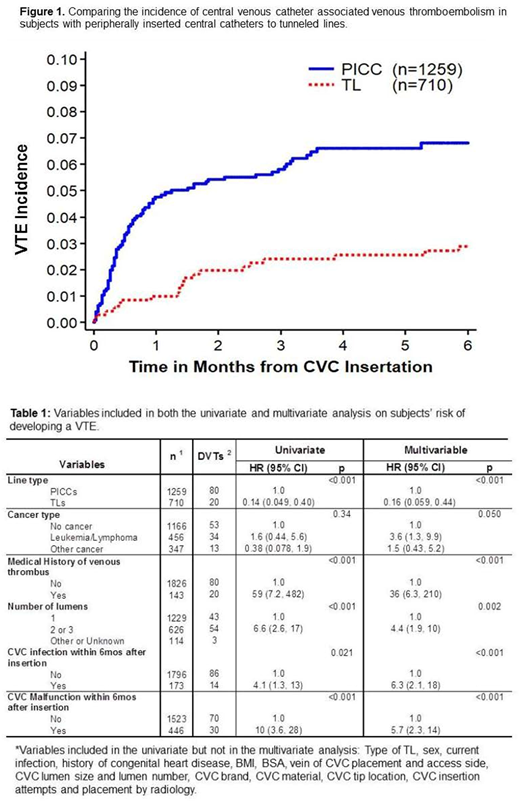
Cumulative incidence rates of VTE, CLABSI, CVC malfunction and removal were estimated and compared between PICCs and TLs. These analyses focused on the first 6 months from CVC insertion using parametric survival models assuming a Weibull survival distribution. The association between occurrence of VTE and subject/CVC characteristics was first assessed in univariate analyses, and then assessed by a minimal multivariable model.
Results
A total of 1,969 CVCs from 1,744 unique patients were included. Median age at CVC insertion was 6.4 years (range: 0.6-17.9) with the majority, 1048 (53%) placed in males. PICCs made up 1,259 (64%) of the CVCs and 710 (36%) were TLs.
Among 1,969 CVCs, 100 had a VTE with a cumulative incidence rate of 5.4±0.5%, and median time to VTE from CVC insertion was 0.6 months (range 0-5.8 months). Eighty percent of the VTEs were in PICCs and median time to VTE was 0.5 months (range 0-5.3 months) in PICCs compared to TLs with a median time to VTE of 1.4 months (range 0-5.8 months). The incidence rate of VTE was 2.9±0.6% for TLs, and 6.8±0.7% for PICCs (Figure 1). In univariate analysis, subjects with TLs had a significantly lower risk of developing a VTE than patients with PICCs (HR=0.14, 95%CI: 0.05-0.4, p<0.001).
The incidence of CLABSI was 14±1.3% for TLs compared to 7.9±0.9% for PICCs and in univariate analysis CVCs with a CLABSI were 4 times (95%CI: 1.3-13) as likely to develop a VTE. The cumulative incidence of malfunction in all CVCs was 25±1.0%, and univariate analysis revealed CVCs with a malfunction were 10 times (95%CI: 3.6, 28) as likely to develop a VTE.
In the multivariable analyses (Table 1), subjects with TLs were significantly less likely to develop a VTE compared to PICCs (HR=0.16, 95%CI: 0.06-0.4, p<0.001); subjects with leukemia were more likely to have a VTE than subjects without cancer or other cancer diagnosis (HR=3.6, 95%CI: 1.3-9.9, p=0.050); subjects with a previous history of VTE were significantly more likely to develop a new VTE (HR=36, 95%CI: 6.3-210, p<0.001); and compared to CVCs with 1 lumen, CVCs with 2-3 lumens resulted in a higher risk of developing a VTE (HR=4.4, 95%CI: 1.9-10, p=0.002). Diagnosis of a CLABSI (HR=6.3, 95%CI: 2.1-18, p<0.001) as well as CVC malfunction (HR=5.7, 95%CI: 2.3-14, p<0.001) were also associated with higher risk of developing a VTE.
Conclusion
This study represents the first prospective evaluation of the incidence and risk factors of VTE for TLs and PICCs placed in children. Almost 2,000 CVCs are included in this final analysis, which revealed a significant increase in VTE risk for children who have a PICC placed compared to a TL. The greatest risk factor for CVC associated VTE was a prior history of VTE. Additional risk factors included CLABSI, CVC malfunction, leukemia and having a multi-lumen CVC.
Even though the ease of placing a PICC is enticing to avoid repeat peripheral intravenous (PIV) insertions or surgical intervention with TL placement, the increased risk of VTE in PICCs should give practitioners pause. When CVC placement is unavoidable, limiting the number of lumens is a modifiable VTE risk factor and efforts to prevent CLABSI may reduce VTE incidence. Interestingly, no insertion characteristics (e.g. placement vein, access side, catheter brand or material, tip location, insertion attempts) were associated with an increased risk of VTE.
Jaffray:Octapharma: Consultancy; CSL Behring: Consultancy, Research Funding; Bayer: Consultancy. Young:Kedrion: Consultancy; Genentech/Roche: Consultancy, Honoraria; CSL Behring: Consultancy, Honoraria; Bioverativ: Consultancy, Honoraria; Bayer: Consultancy; Novo Nordisk: Consultancy, Honoraria; Shire: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal